Top Surgery
Top Surgery
Top Surgery or Gender Masculinisation Surgery
Surgical procedures aimed at masculinization, known as gender-affirming or gender-confirmation surgery are undertaken to align an individual's physical characteristics with their gender identity. These surgeries encompass various options, including chest masculinization to achieve a more typically male chest contour.
Understanding Top Surgery
Top surgery, often known as chest masculinisation surgery, is a procedure designed to remove breast tissue (mastectomy) and reshape the nipples and chest, aiming to achieve a more masculine appearance for transgender and nonbinary individuals.
Just as gender identity varies, so do preferences in top surgery outcomes. Patients may desire anything from a completely flat chest to a more subtle reduction in breast size.
The primary reason for top surgery is to assist the patient with gender affirmation, however cosmetic outcome is also an important factor to surgical success. There are a number of different types of top surgery and within those procedures different techniques used to provide the best final outcome.
The two most common types of top surgery are Double Incision Mastectomy and Single Incision Mastectomy also know as Minimally Invasive or Peri-Areolar Mastectomy.
Indications for Top Surgery
Transgender and nonbinary people may require top surgery as part of their gender affirmation journey. Top surgery can be part of a person’s affirmation surgery plan to address gender dysphoria, which occurs when gender identity does not correspond to the person’s birth sex.
Gender affirmation surgery, including chest masculinization procedures, can improve well-being in patients who:
Have ongoing and documented gender dysphoria.
Have the competency to make responsible medical decisions for themselves.
Have successfully addressed other mental and physical health concerns.
"Breast Cancer is the most common cancer in the world. Australia has some of the highest rates of breast cancer with 1 in 7 women affected by breast cancer in their lifetime."
Top Surgery, Breast Disease and Breast Cancer
Throughout the pre-clinic questionnaire and consultation process, information will be taken that may initially appear unrelated to top surgery. However, these questions are crucial for the surgeon to evaluate your risk factors for breast cancer. Additionally, prior to undergoing top surgery, you will undergo one or more scans to rule out any pre-existing pathology. The selection of scan types will be determined based on factors such as age, medical history, and findings from physical examinations.
The approach taken by a breast surgeon varies significantly depending on how healthy the breasts are including if cancer is detected. Proceeding with top surgery without assessing the underlying health of the breast including the absence of cancer, can significantly and irreversibly impact cancer treatment outcomes.
If cancer or other diseases are detected, there are treatment protocols that need to be taken prior to surgery to ensure the best outcome. This does not mean that surgery can not be performed, but it does change the sequence and type of surgery to ensure the cancer is treated effectively.
It is important that the surgeon conducting any type of breast surgery remain informed of the evolving landscape of breast cancer management options. Breast surgeons with Oncoplastic specialisation are best trained to manage this type of issue.
Types of Top Surgery
While various surgical techniques are available for top surgery, two primary types of procedures are commonly performed. These include the single and double incision mastectomies which are suitable for the majority of individuals and typically yield optimal surgical and cosmetic results. Other less common techniques are employed infrequently and are reserved for specific body types.

Double Incision Mastectomy
Double incision mastectomy is the most common top surgery option. It can remove the most breast tissue and allows scars to be placed in a more masculine position to enhance chest contour.
You can read more about the double incision mastectomy here.

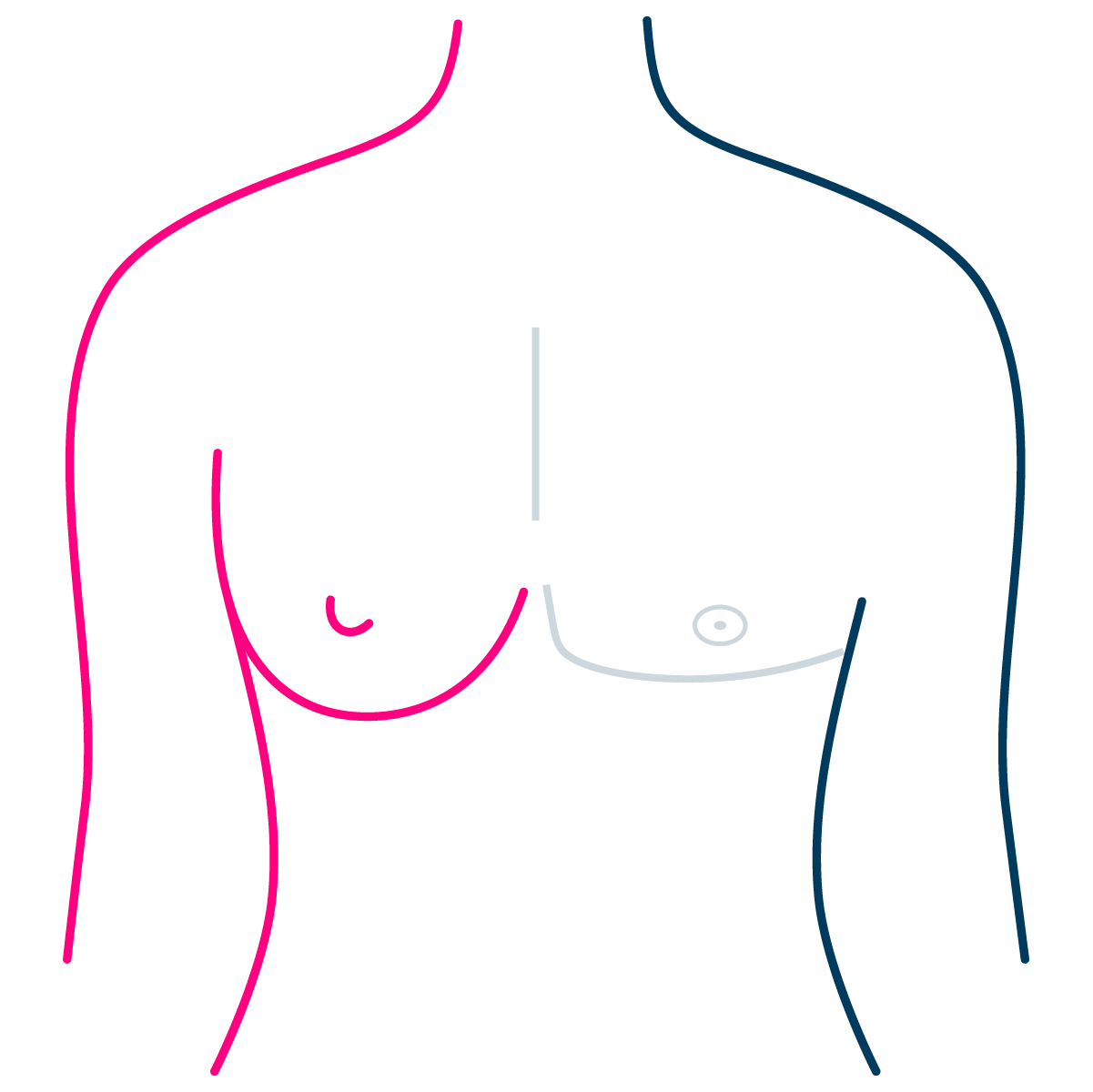
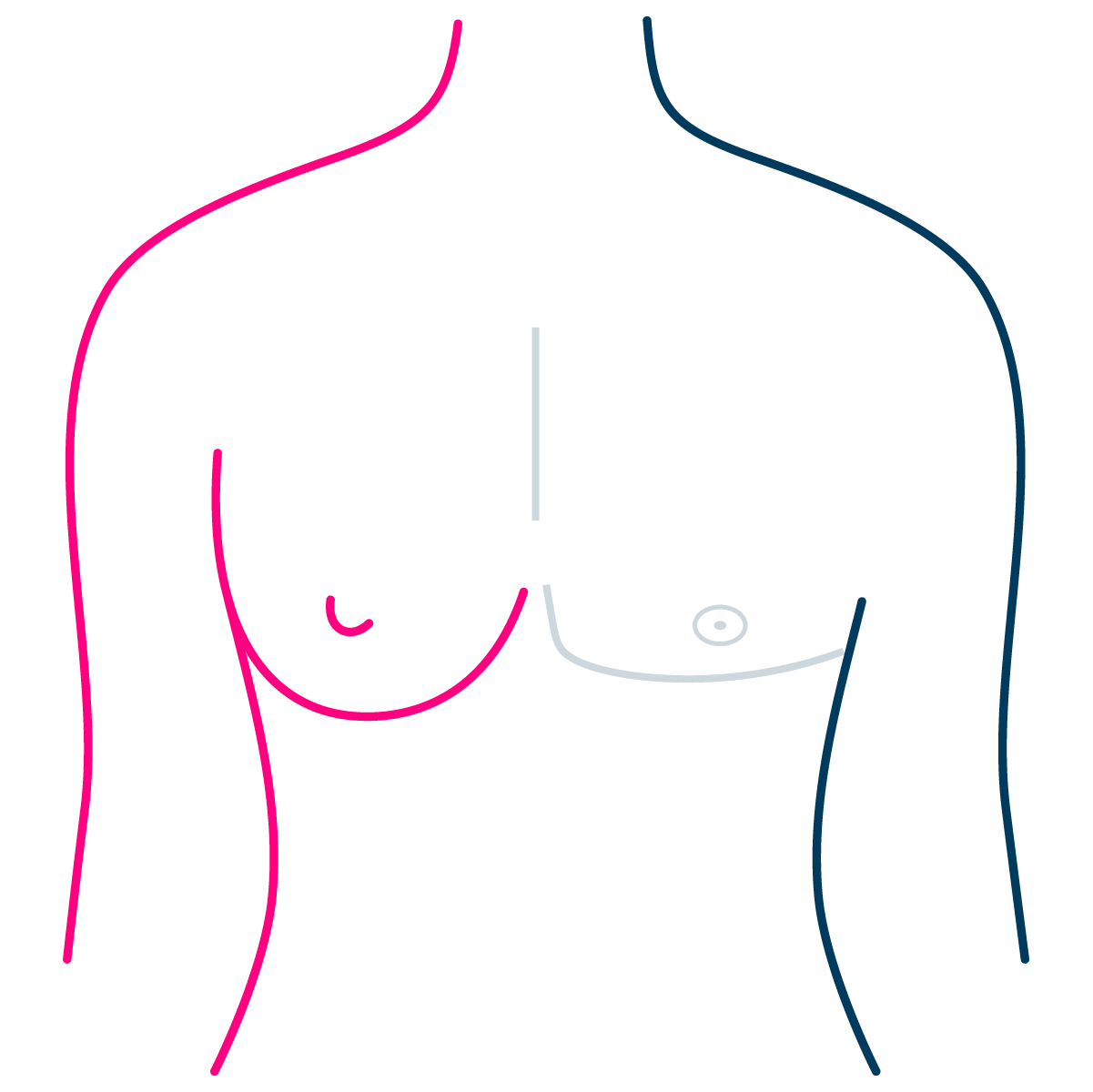
Single Incision Mastectomy
Single incision mastectomy is also known as minimally invasive or peri-areolar mastectomy. Single incision mastectomy is suitable for people with smaller breasts. It has the benefit of minimal scar, keeping your own nipple and a higher possibility of retaining nipple sensation.
You can read more about the single incision mastectomy here.

Breast Reduction Surgery
In certain cases, individuals may opt to preserve some degree of femininity by retaining a breast mound. Breast reduction surgery may be deemed more suitable in such instances.
Typically, it is feasible to preserve the nipple along with its own blood supply during breast reduction surgery. However, if the disparity in size between the original breast and the desired breast is considerable, it may be necessary to remove the nipple similar to a double incision mastectomy. In such cases, the nipple may be replaced with a free nipple graft or tattoo.
In highly specific situations, several alternative approaches may be considered based on individual body type and desired aesthetic outcomes. Given the unique nature of each individual, it is advisable to bring along reference photos depicting your desired appearance to facilitate a thorough discussion with the surgeon.
Patient Underlying Health and Consent
Before undergoing surgery, your surgeon will engage in discussions regarding your desired surgical outcome and will conduct a comprehensive review of your medical history. An essential component of this process involves obtaining informed consent, wherein the risks and potential outcomes of the planned surgery are thoroughly discussed and acknowledged.
Body Composition and Weight
A patient’s weight is not a limiting factor for undergoing surgery, however, there are a few considerations for all patients wishing to undergo top surgery.
In the transgender community, BMI and weight are often used as additional barriers for patients to overcome before receiving the required surgery.
Normally, when assessing any patient for surgery, an above average BMI (patients who are holding more relative weight to their height) may be at higher risk of anaesthetic complication during the surgery. Higher BMI is also associated with slower wound healing and higher chance of infection.
However, a small study conducted in 2021 on transgender patients demonstrates similar surgical outcomes irrespective of BMI and weight.
All of the techniques used for top surgery are custom-tailored to accommodate your unique body shape. Individuals with larger breasts and excess tissue under their arms may necessitate adjustments to surgical approach to ensure the best aesthetic outcome.
These considerations should not dissuade a surgeon from providing you with the necessary surgery to meet your needs.
Age of Consent
Regarding aesthetic outcomes, it is generally observed that individuals who commence gender affirming treatment at a younger age tend to achieve more favorable results. This may translate to requiring less invasive surgical procedures and yielding superior cosmetic outcomes. However, the age at which patients can provide informed consent for gender affirming treatment remains a subject of considerable debate.
In Australia, health practitioners are bound by law when offering gender affirmation surgery as the procedure is irreversible.
Currently everyone who wishes to have gender affirmation surgery will require a completed WPATH assessment by a psychologist. Your WPATH does not expire as long as you have not changed your mind.
Prior to undergoing gender affirming surgery, consent will need to be obtained from the following people:
Adults above 18 who are deemed competent to make their treatment decisions can provide consent for surgery independently.
Individuals between the ages of 16 and 18 will require signatures from all parties with parental responsibilities (e.g., both parents or legal guardians) in addition to their own consent.
Children younger than 16, as well as those whose parents/legal guardians are unable to reach an agreement, will need family court approval before undergoing surgery. Alternatively, they may choose to defer surgery until they reach the age of 18.
This is an ever-changing area, we remain reactive to changes in legislation.
Prior to your appointment
A/Prof Tsao is experienced at performing all of the above surgical techniques, and is a member of the LGBTQIA+ community. During an appointment you are encouraged to discuss your surgical and cosmetic preferences openly.
To help you get the most out of your consultation, we recommend completing the following prior to your appointment:
Search online for other examples of top surgery, and collect some pictures of your desired cosmetic outcome. Consider your current body type and those in the pictures. Try to choose examples that have a similar body type to you. These will be a good benchmark for discussion with your surgeon.
During your consultation, the final contour of the chest, nipple type, nipple placement and overall aesthetic will be discussed. Considering each of these areas prior to the consult can help you feel confident during the conversation. It is important during this conversation that you have an open mind as to outcome, as there may be some types of surgery or techniques that may not yield strong results for your body type.
Consider bringing an support person to your consultation. If you are under the age of 18, a parent or legal guardian is encouraged to attend.
Prepare any questions you may have for during the appointment.
When you are ready, you can make an appointment here.
Links to Additional Information
Appointment booking is provided in English.
Consultations are provided in English and Mandarin Chinese.